Disability Tax Credit Application - Fill, Sign Online, Download & Print - No Signup
Protected B
when completed
Help
canada.ca/disability
-tax-credit
1-800-959-8281
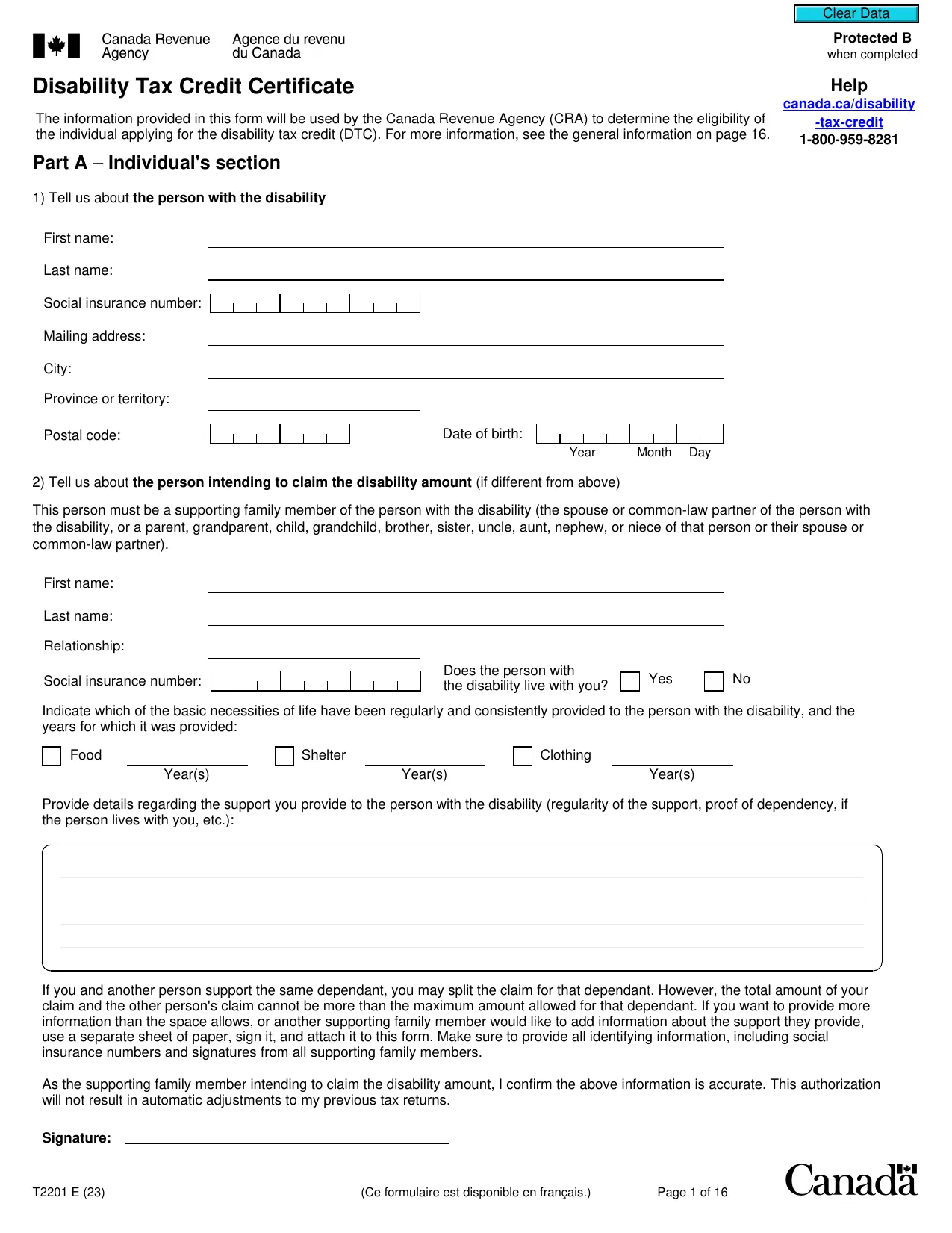
Disability Tax Credit Certificate
The information provided in this form will be used by the Canada Revenue Agency (CRA) to determine the eligibility of
the individual applying for the disability tax credit (DTC). For more information, see the general information on page 16.
Part A
–
Individual's section
1) Tell us about
the person with the disability
First name:
Last name:
Social insurance number:
Mailing address:
City:
Province or territory:
Postal code:
Date of birth:
Year Month Day
2) Tell us about
the person intending to claim the disability amount
(if different from above)
This person must be a supporting family member of the person with the disability (the spouse or common-law partner of the person with
the disability, or a parent, grandparent, child, grandchild, brother, sister, uncle, aunt, nephew, or niece of that person or their spouse or
common-law partner).
First name:
Last name:
Relationship:
Social insurance number:
Does the person with
the disability live with you?
Yes
No
Indicate which of the basic necessities of life have been regularly and consistently provided to the person with the disability, and the
years for which it was provided:
Food
Year(s)
Shelter
Year(s)
Clothing
Year(s)
Provide details regarding the support you provide to the person with the disability (regularity of the support, proof of dependency, if
the person lives with you, etc.):
If you and another person support the same dependant, you may split the claim for that dependant. However, the total amount of your
claim and the other person's claim cannot be more than the maximum amount allowed for that dependant. If you want to provide more
information than the space allows, or another supporting family member would like to add information about the support they provide,
use a separate sheet of paper, sign it, and attach it to this form. Make sure to provide all identifying information, including social
insurance numbers and signatures from all supporting family members.
As the supporting family member intending to claim the disability amount, I confirm the above information is accurate. This authorization
will not result in automatic adjustments to my previous tax returns.
Signature:
T2201 E (23)
(Ce formulaire est disponible en français.)
Page 1 of 16
Clear Data
Protected B
when completed
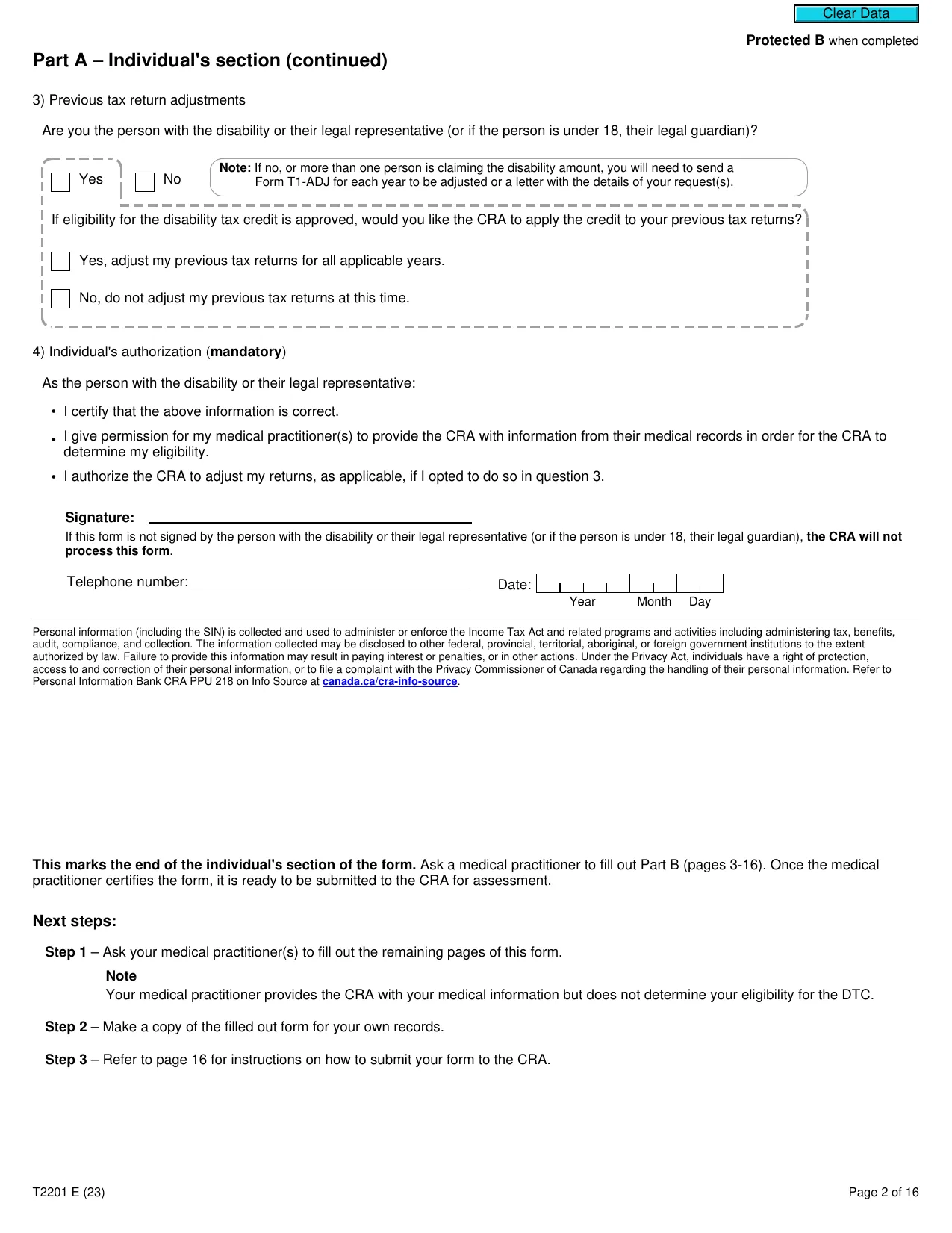
Part A
–
Individual's section (continued)
3) Previous tax return adjustments
Are you the person with the disability or their legal representative (or if the person is under 18, their legal guardian)?
Note:
If no, or more than one person is claiming the disability amount, you will need to send a
Form T1-ADJ for each year to be adjusted or a letter with the details of your request(s).
Yes
No
If eligibility for the disability tax credit is approved, would you like the CRA to apply the credit to your previous tax returns?
Yes, adjust my previous tax returns for all applicable years.
No, do not adjust my previous tax returns at this time.
4) Individual's authorization (
mandatory
)
As the person with the disability or their legal representative:
• I certify that the above information is correct.
•
I give permission for my medical practitioner(s) to provide the CRA with information from their medical records in order for the CRA to
determine my eligibility.
• I authorize the CRA to adjust my returns, as applicable, if I opted to do so in question 3.
Signature:
If this form is not signed by the person with the disability or their legal representative (or if the person is under 18, their legal guardian),
the CRA will not
process this form
.
Telephone number:
Date:
Year Month Day
Personal information (including the SIN) is collected and used to administer or enforce the Income Tax Act and related programs and activities including administering tax, benefits,
audit, compliance, and collection. The information collected may be disclosed to other federal, provincial, territorial, aboriginal, or foreign government institutions to the extent
authorized by law. Failure to provide this information may result in paying interest or penalties, or in other actions. Under the Privacy Act, individuals have a right of protection,
access to and correction of their personal information, or to file a complaint with the Privacy Commissioner of Canada regarding the handling of their personal information. Refer to
Personal Information Bank CRA PPU 218 on Info Source at
canada.ca/cra-info-source
.
This marks the end of the individual's section of the form.
Ask a medical practitioner to fill out Part B (pages 3-16). Once the medical
practitioner certifies the form, it is ready to be submitted to the CRA for assessment.
Next steps:
Step 1
– Ask your medical practitioner(s) to fill out the remaining pages of this form.
Note
Your medical practitioner provides the CRA with your medical information but does not determine your eligibility for the DTC.
Step 2
– Make a copy of the filled out form for your own records.
Step 3
– Refer to page 16 for instructions on how to submit your form to the CRA.
T2201 E (23)
Page 2 of 16
Clear Data
Protected B
when completed
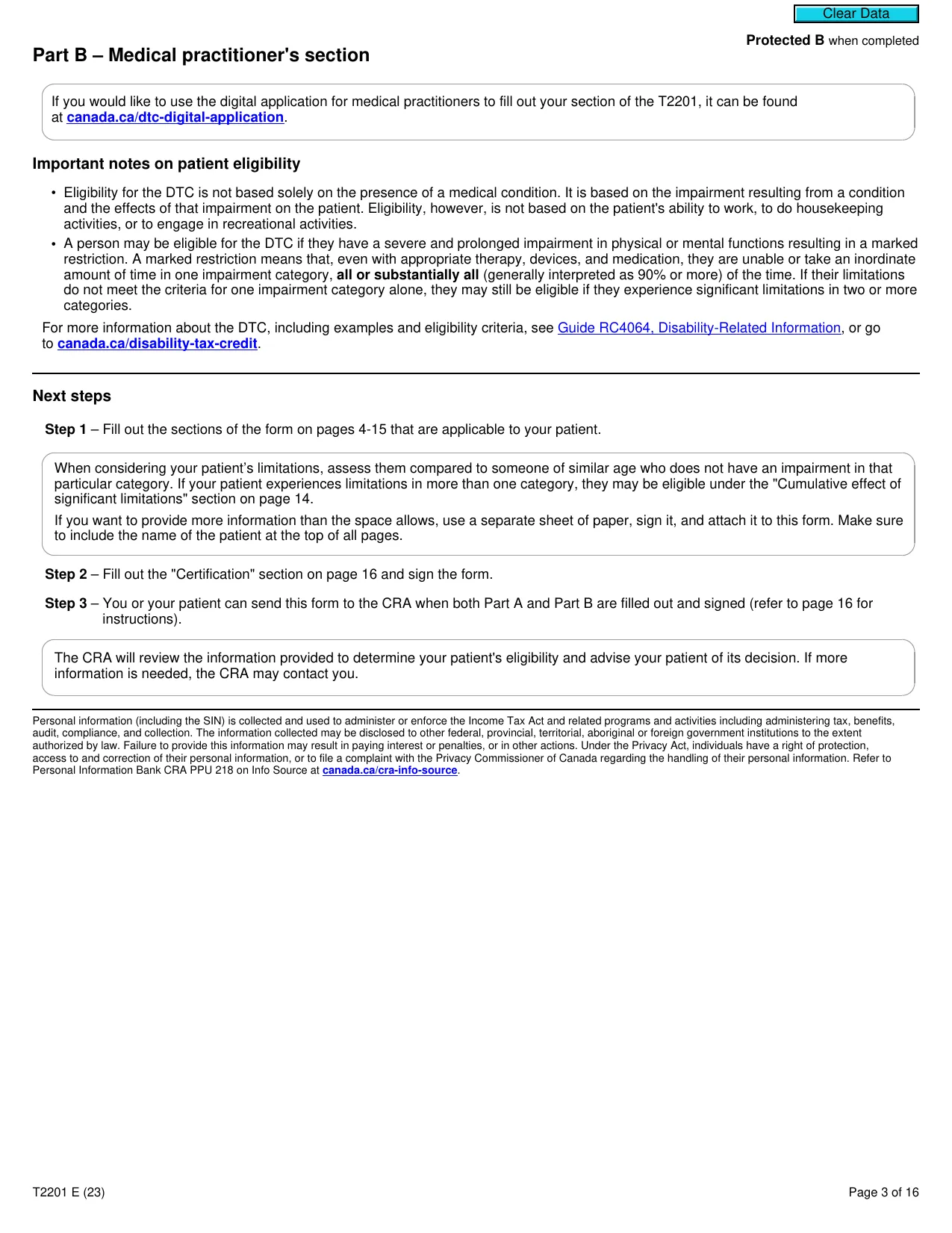
Part B – Medical practitioner's section
If you would like to use the digital application for medical practitioners to fill out your section of the T2201, it can be found
at
canada.ca/dtc-digital-application
.
Important notes on patient eligibility
• Eligibility for the DTC is not based solely on the presence of a medical condition. It is based on the impairment resulting from a condition
and the effects of that impairment on the patient. Eligibility, however, is not based on the patient's ability to work, to do housekeeping
activities, or to engage in recreational activities.
• A person may be eligible for the DTC if they have a severe and prolonged impairment in physical or mental functions resulting in a marked
restriction. A marked restriction means that, even with appropriate therapy, devices, and medication, they are unable or take an inordinate
amount of time in one impairment category,
all or substantially all
(generally interpreted as 90% or more) of the time. If their limitations
do not meet the criteria for one impairment category alone, they may still be eligible if they experience significant limitations in two or more
categories.
For more information about the DTC, including examples and eligibility criteria, see
Guide RC4064, Disability-Related Information
, or go
to
canada.ca/disability-tax-credit
.
Next steps
Step 1
– Fill out the sections of the form on pages 4-15 that are applicable to your patient.
When considering your patient’s limitations, assess them compared to someone of similar age who does not have an impairment in that
particular category. If your patient experiences limitations in more than one category, they may be eligible under the "Cumulative effect of
significant limitations" section on page 14.
If you want to provide more information than the space allows, use a separate sheet of paper, sign it, and attach it to this form. Make sure
to include the name of the patient at the top of all pages.
Step 2
– Fill out the "Certification" section on page 16 and sign the form.
Step 3
– You or your patient can send this form to the CRA when both Part A and Part B are filled out and signed (refer to page 16 for
instructions).
The CRA will review the information provided to determine your patient's eligibility and advise your patient of its decision. If more
information is needed, the CRA may contact you.
Personal information (including the SIN) is collected and used to administer or enforce the Income Tax Act and related programs and activities including administering tax, benefits,
audit, compliance, and collection. The information collected may be disclosed to other federal, provincial, territorial, aboriginal or foreign government institutions to the extent
authorized by law. Failure to provide this information may result in paying interest or penalties, or in other actions. Under the Privacy Act, individuals have a right of protection,
access to and correction of their personal information, or to file a complaint with the Privacy Commissioner of Canada regarding the handling of their personal information. Refer to
Personal Information Bank CRA PPU 218 on Info Source at
canada.ca/cra-info-source
.
T2201 E (23)
Page 3 of 16
Clear Data
Protected B
when completed
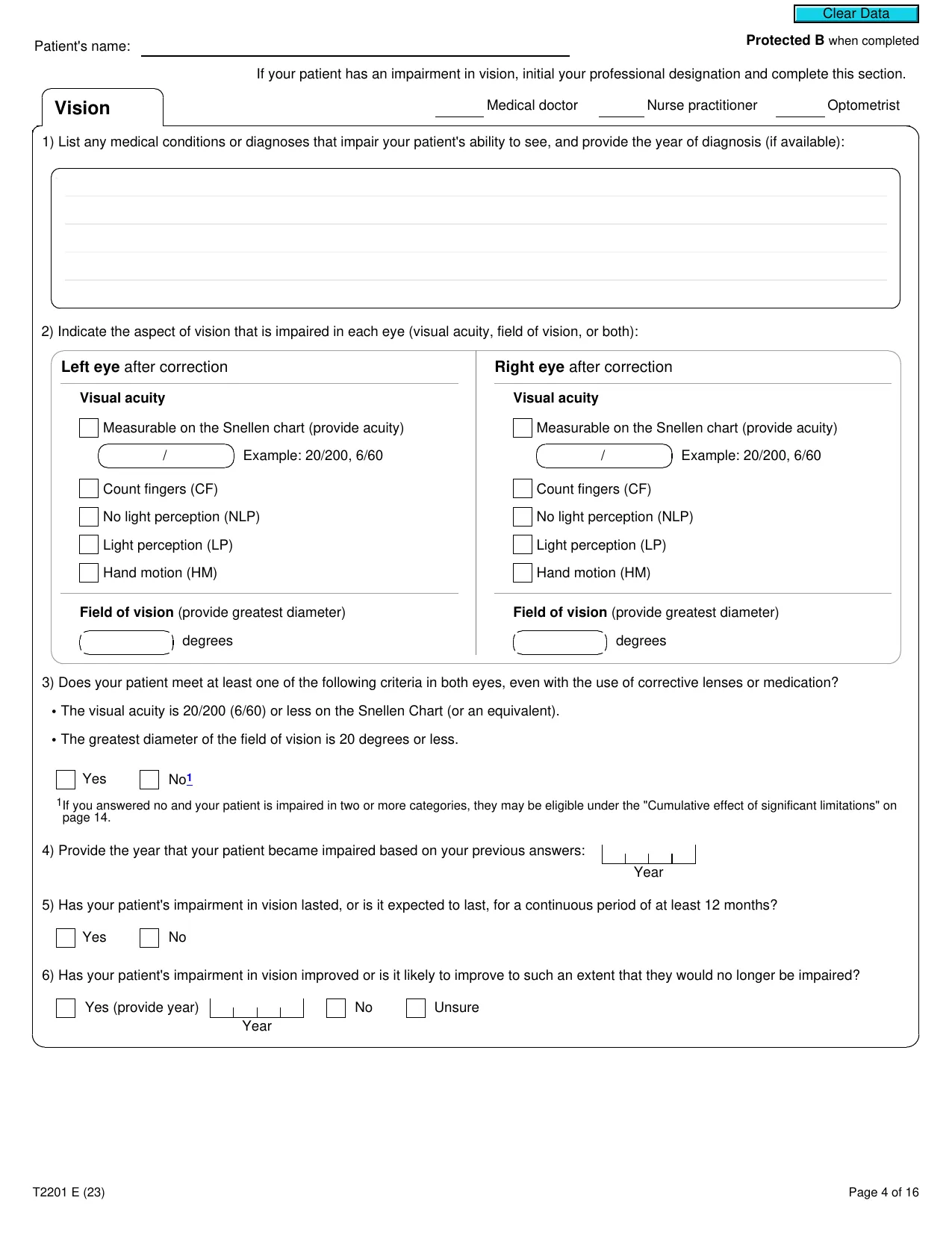
Patient's name:
If your patient has an impairment in vision, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Optometrist
Vision
1) List any medical conditions or diagnoses that impair your patient's ability to see, and provide the year of diagnosis (if available):
2) Indicate the aspect of vision that is impaired in each eye (visual acuity, field of vision, or both):
Left eye
after correction
Visual acuity
Measurable on the Snellen chart (provide acuity)
/
Example: 20/200, 6/60
Count fingers (CF)
No light perception (NLP)
Light perception (LP)
Hand motion (HM)
Field of vision
(provide greatest diameter)
degrees
Right eye
after correction
Visual acuity
Measurable on the Snellen chart (provide acuity)
/
Example: 20/200, 6/60
Count fingers (CF)
No light perception (NLP)
Light perception (LP)
Hand motion (HM)
Field of vision
(provide greatest diameter)
degrees
3) Does your patient meet at least one of the following criteria in both eyes, even with the use of corrective lenses or medication?
• The visual acuity is 20/200 (6/60) or less on the Snellen Chart (or an equivalent).
• The greatest diameter of the field of vision is 20 degrees or less.
Yes
No
1
1
If you answered no and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
4) Provide the year that your patient became impaired based on your previous answers:
Year
5) Has your patient's impairment in vision lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
6) Has your patient's impairment in vision improved or is it likely to improve to such an extent that they would no longer be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 4 of 16
Clear Data
Protected B
when completed
Patient's name:
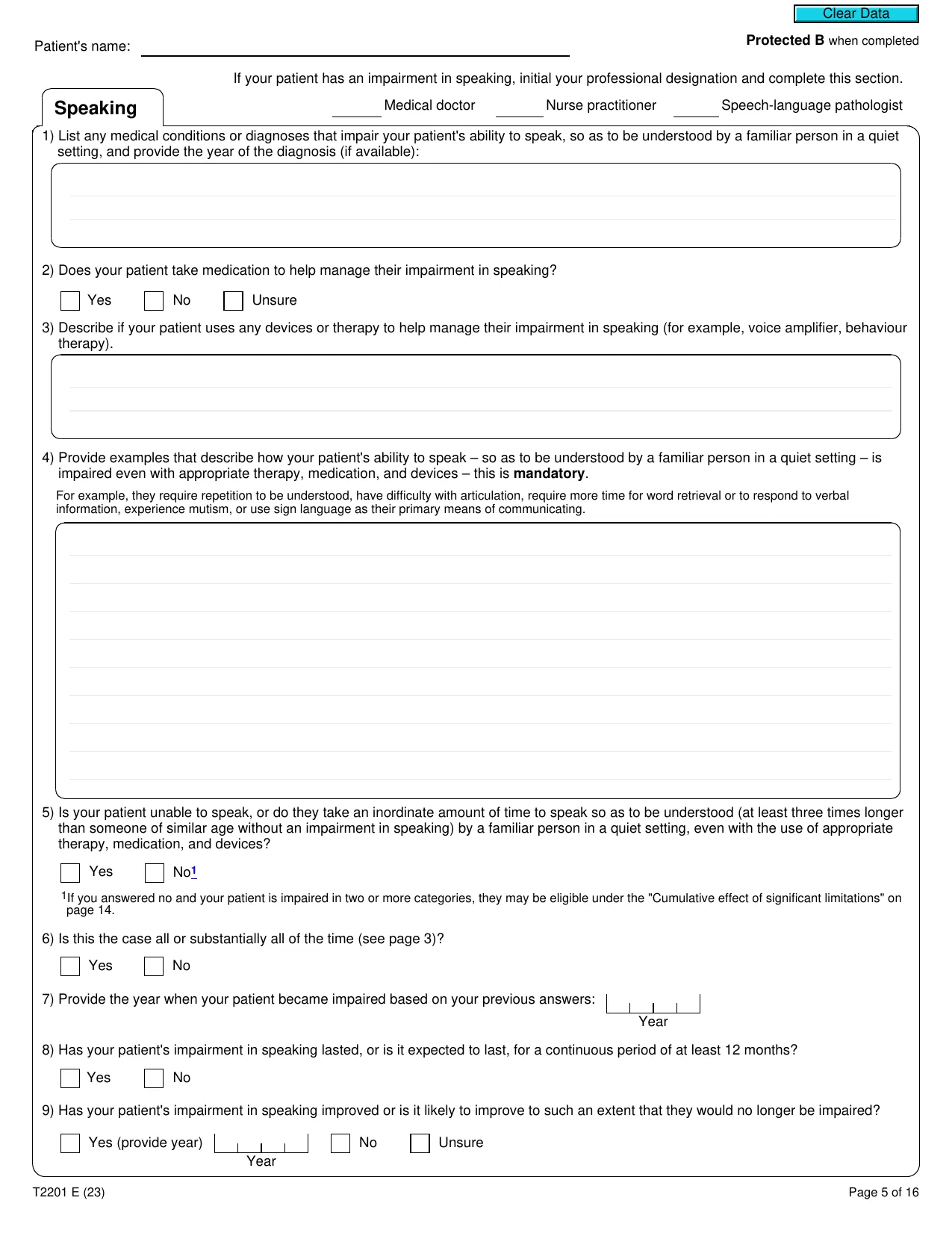
If your patient has an impairment in speaking, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Speech-language pathologist
Speaking
1) List any medical conditions or diagnoses that impair your patient's ability to speak, so as to be understood by a familiar person in a quiet
setting, and provide the year of the diagnosis (if available):
2) Does your patient take medication to help manage their impairment in speaking?
Yes
No
Unsure
3) Describe if your patient uses any devices or therapy to help manage their impairment in speaking (for example, voice amplifier, behaviour
therapy).
4) Provide examples that describe how your patient's ability to speak – so as to be understood by a familiar person in a quiet setting – is
impaired even with appropriate therapy, medication, and devices – this is
mandatory
.
For example, they require repetition to be understood, have difficulty with articulation, require more time for word retrieval or to respond to verbal
information, experience mutism, or use sign language as their primary means of communicating.
5) Is your patient unable to speak, or do they take an inordinate amount of time to speak so as to be understood (at least three times longer
than someone of similar age without an impairment in speaking) by a familiar person in a quiet setting, even with the use of appropriate
therapy, medication, and devices?
Yes
No
1
1
If you answered no and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in speaking lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in speaking improved or is it likely to improve to such an extent that they would no longer be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 5 of 16
Clear Data
Protected B
when completed
Patient's name:
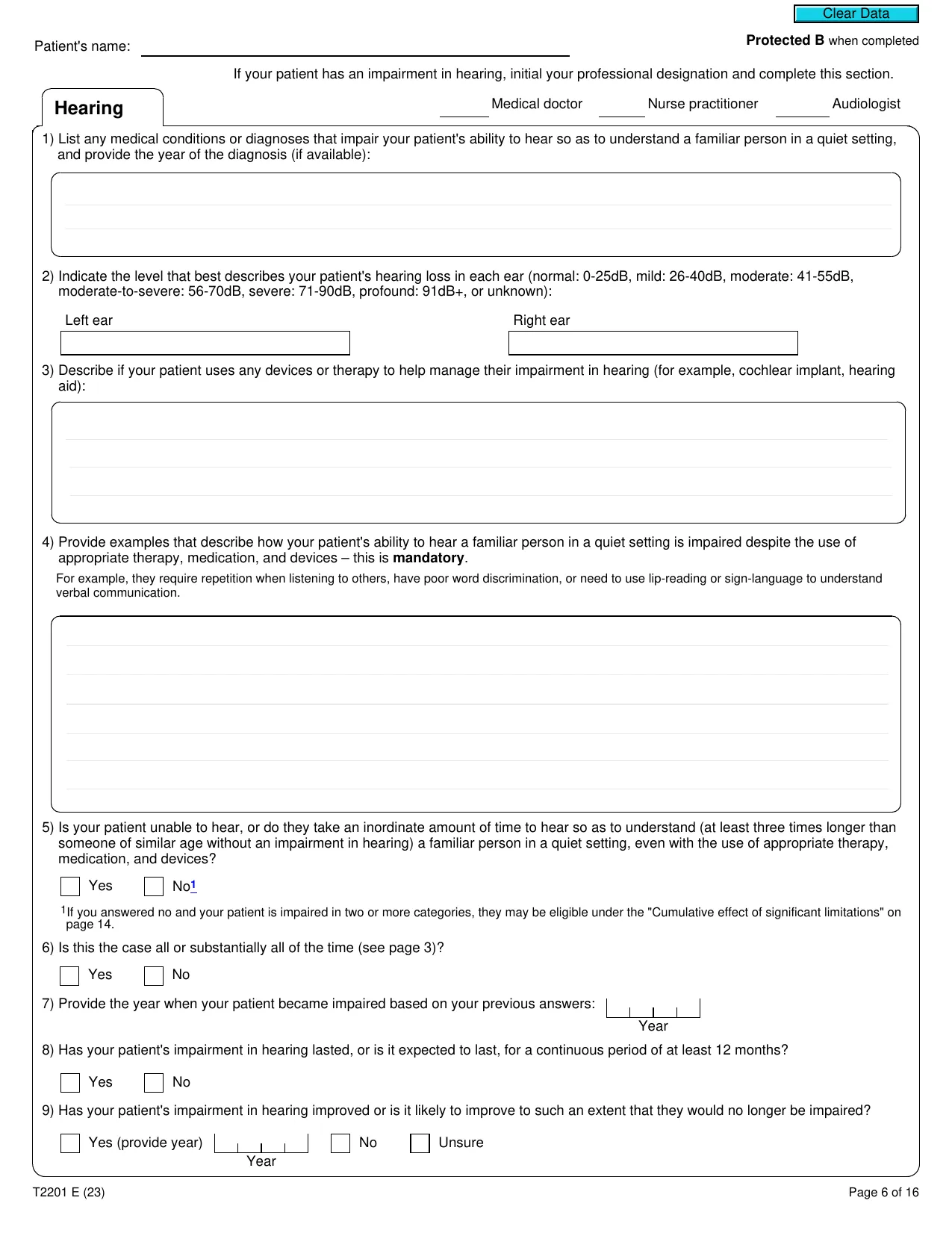
If your patient has an impairment in hearing, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Audiologist
Hearing
1) List any medical conditions or diagnoses that impair your patient's ability to hear so as to understand a familiar person in a quiet setting,
and provide the year of the diagnosis (if available):
2) Indicate the level that best describes your patient's hearing loss in each ear (normal: 0-25dB, mild: 26-40dB, moderate: 41-55dB,
moderate-to-severe: 56-70dB, severe: 71-90dB, profound: 91dB+, or unknown):
Left ear
Right ear
3) Describe if your patient uses any devices or therapy to help manage their impairment in hearing (for example, cochlear implant, hearing
aid):
4) Provide examples that describe how your patient's ability to hear a familiar person in a quiet setting is impaired despite the use of
appropriate therapy, medication, and devices – this is
mandatory
.
For example, they require repetition when listening to others, have poor word discrimination, or need to use lip-reading or sign-language to understand
verbal communication.
5) Is your patient unable to hear, or do they take an inordinate amount of time to hear so as to understand (at least three times longer than
someone of similar age without an impairment in hearing) a familiar person in a quiet setting, even with the use of appropriate therapy,
medication, and devices?
Yes
No
1
1
If you answered no and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in hearing lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in hearing improved or is it likely to improve to such an extent that they would no longer be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 6 of 16
Clear Data
Protected B
when completed
Patient's name:
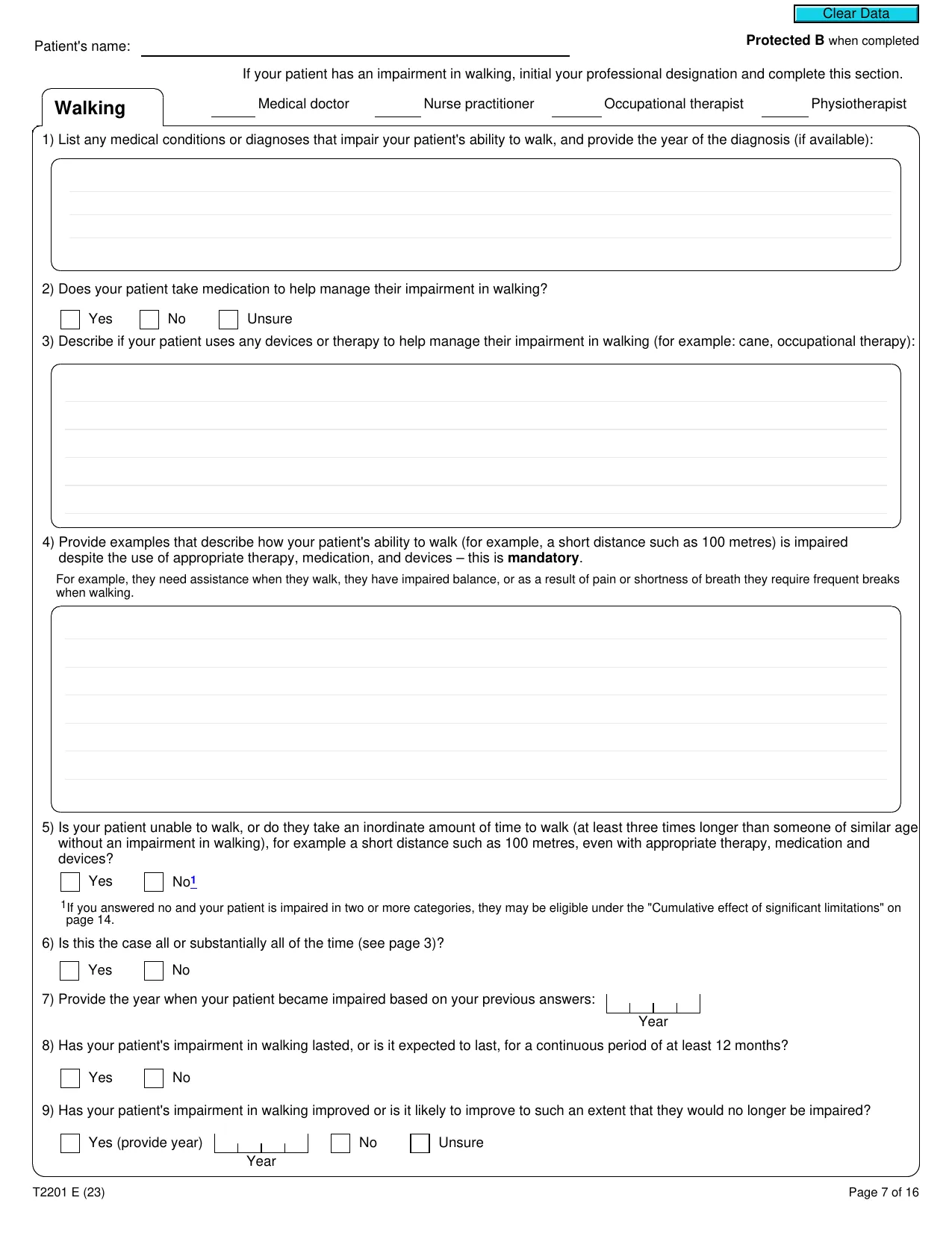
If your patient has an impairment in walking, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Occupational therapist
Physiotherapist
Walking
1) List any medical conditions or diagnoses that impair your patient's ability to walk, and provide the year of the diagnosis (if available):
2) Does your patient take medication to help manage their impairment in walking?
Yes
No
Unsure
3) Describe if your patient uses any devices or therapy to help manage their impairment in walking (for example: cane, occupational therapy):
4) Provide examples that describe how your patient's ability to walk (for example, a short distance such as 100 metres) is impaired
despite the use of appropriate therapy, medication, and devices – this is
mandatory
.
For example, they need assistance when they walk, they have impaired balance, or as a result of pain or shortness of breath they require frequent breaks
when walking.
5) Is your patient unable to walk, or do they take an inordinate amount of time to walk (at least three times longer than someone of similar age
without an impairment in walking), for example a short distance such as 100 metres, even with appropriate therapy, medication and
devices?
Yes
No
1
1
If you answered no and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in walking lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in walking improved or is it likely to improve to such an extent that they would no longer be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 7 of 16
Clear Data
Protected B
when completed
Patient's name:
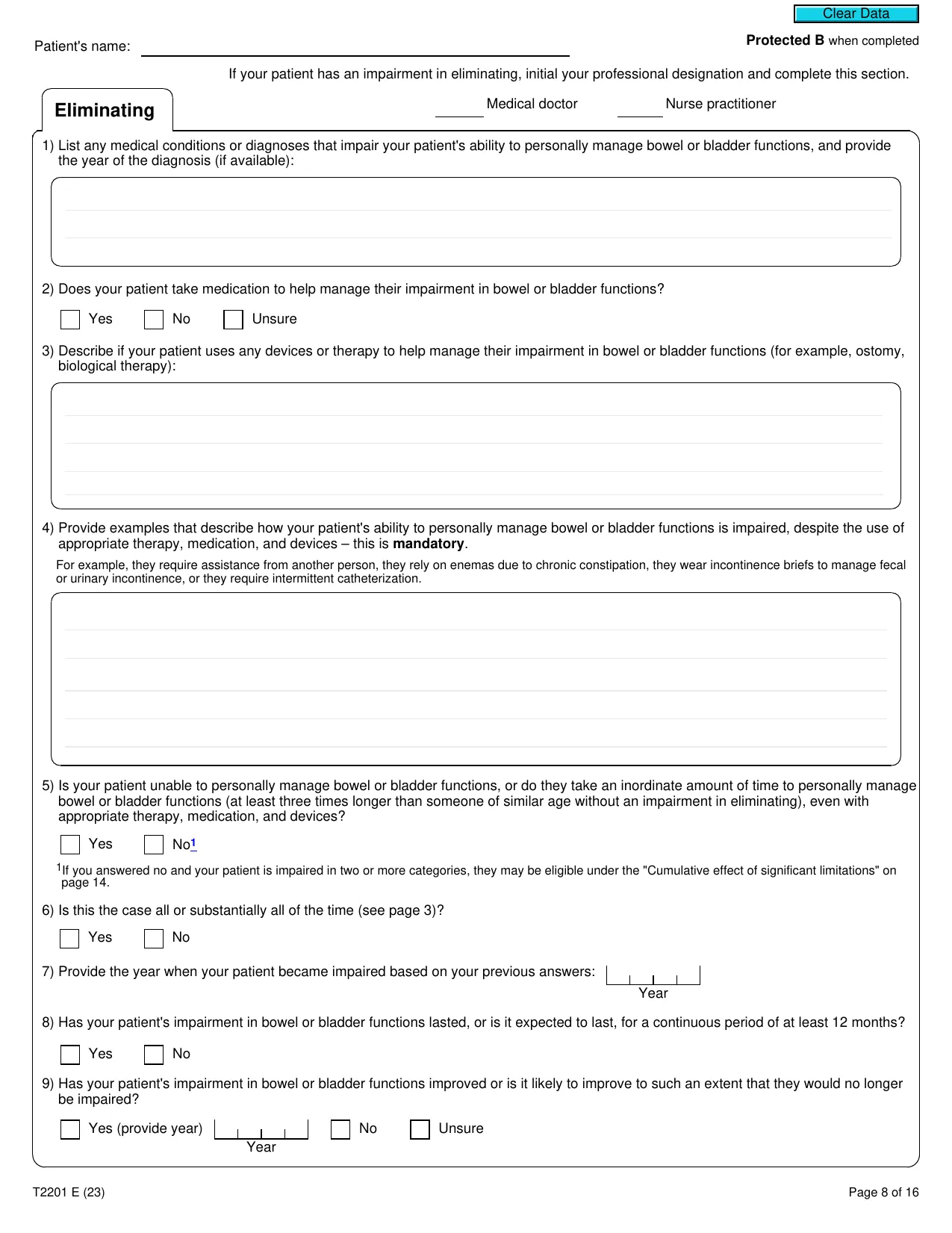
If your patient has an impairment in eliminating, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Eliminating
1) List any medical conditions or diagnoses that impair your patient's ability to personally manage bowel or bladder functions, and provide
the year of the diagnosis (if available):
2) Does your patient take medication to help manage their impairment in bowel or bladder functions?
Yes
No
Unsure
3) Describe if your patient uses any devices or therapy to help manage their impairment in bowel or bladder functions (for example, ostomy,
biological therapy):
4) Provide examples that describe how your patient's ability to personally manage bowel or bladder functions is impaired, despite the use of
appropriate therapy, medication, and devices – this is
mandatory
.
For example, they require assistance from another person, they rely on enemas due to chronic constipation, they wear incontinence briefs to manage fecal
or urinary incontinence, or they require intermittent catheterization.
5) Is your patient unable to personally manage bowel or bladder functions, or do they take an inordinate amount of time to personally manage
bowel or bladder functions (at least three times longer than someone of similar age without an impairment in eliminating), even with
appropriate therapy, medication, and devices?
Yes
No
1
1
If you answered no and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in bowel or bladder functions lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in bowel or bladder functions improved or is it likely to improve to such an extent that they would no longer
be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 8 of 16
Clear Data
Protected B
when completed
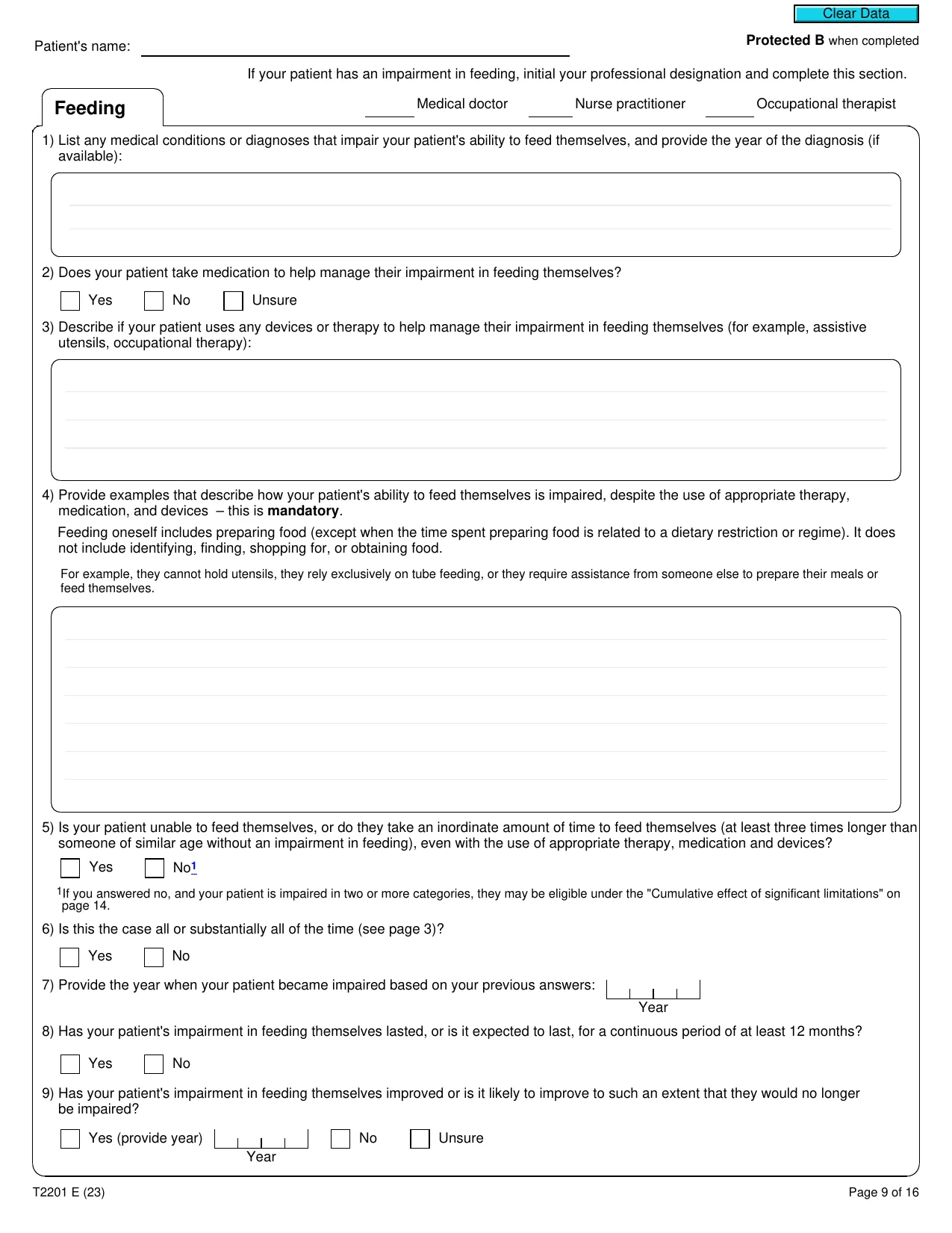
Patient's name:
If your patient has an impairment in feeding, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Occupational therapist
Feeding
1) List any medical conditions or diagnoses that impair your patient's ability to feed themselves, and provide the year of the diagnosis (if
available):
2) Does your patient take medication to help manage their impairment in feeding themselves?
Yes
No
Unsure
3) Describe if your patient uses any devices or therapy to help manage their impairment in feeding themselves (for example, assistive
utensils, occupational therapy):
4) Provide examples that describe how your patient's ability to feed themselves is impaired, despite the use of appropriate therapy,
medication, and devices – this is
mandatory
.
Feeding oneself includes preparing food (except when the time spent preparing food is related to a dietary restriction or regime). It does
not include identifying, finding, shopping for, or obtaining food.
For example, they cannot hold utensils, they rely exclusively on tube feeding, or they require assistance from someone else to prepare their meals or
feed themselves.
5) Is your patient unable to feed themselves, or do they take an inordinate amount of time to feed themselves (at least three times longer than
someone of similar age without an impairment in feeding), even with the use of appropriate therapy, medication and devices?
Yes
No
1
1
If you answered no, and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in feeding themselves lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in feeding themselves improved or is it likely to improve to such an extent that they would no longer
be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 9 of 16
Clear Data
Protected B
when completed
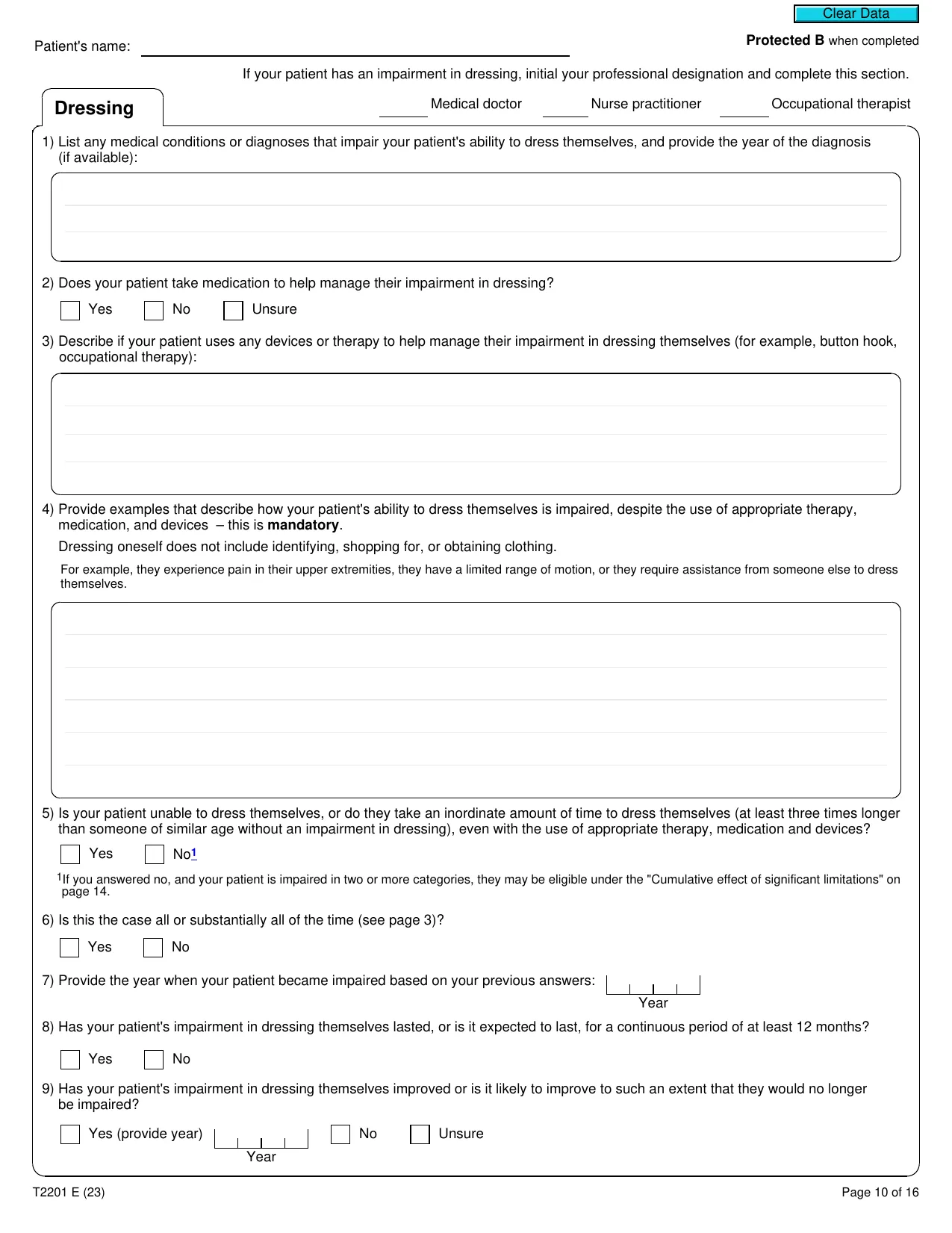
Patient's name:
If your patient has an impairment in dressing, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Occupational therapist
Dressing
1) List any medical conditions or diagnoses that impair your patient's ability to dress themselves, and provide the year of the diagnosis
(if available):
2) Does your patient take medication to help manage their impairment in dressing?
Yes
No
Unsure
3) Describe if your patient uses any devices or therapy to help manage their impairment in dressing themselves (for example, button hook,
occupational therapy):
4) Provide examples that describe how your patient's ability to dress themselves is impaired, despite the use of appropriate therapy,
medication, and devices – this is
mandatory
.
Dressing oneself does not include identifying, shopping for, or obtaining clothing.
For example, they experience pain in their upper extremities, they have a limited range of motion, or they require assistance from someone else to dress
themselves.
5) Is your patient unable to dress themselves, or do they take an inordinate amount of time to dress themselves (at least three times longer
than someone of similar age without an impairment in dressing), even with the use of appropriate therapy, medication and devices?
Yes
No
1
1
If you answered no, and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
6) Is this the case all or substantially all of the time (see page 3)?
Yes
No
7) Provide the year when your patient became impaired based on your previous answers:
Year
8) Has your patient's impairment in dressing themselves lasted, or is it expected to last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment in dressing themselves improved or is it likely to improve to such an extent that they would no longer
be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 10 of 16
Clear Data
Protected B
when completed
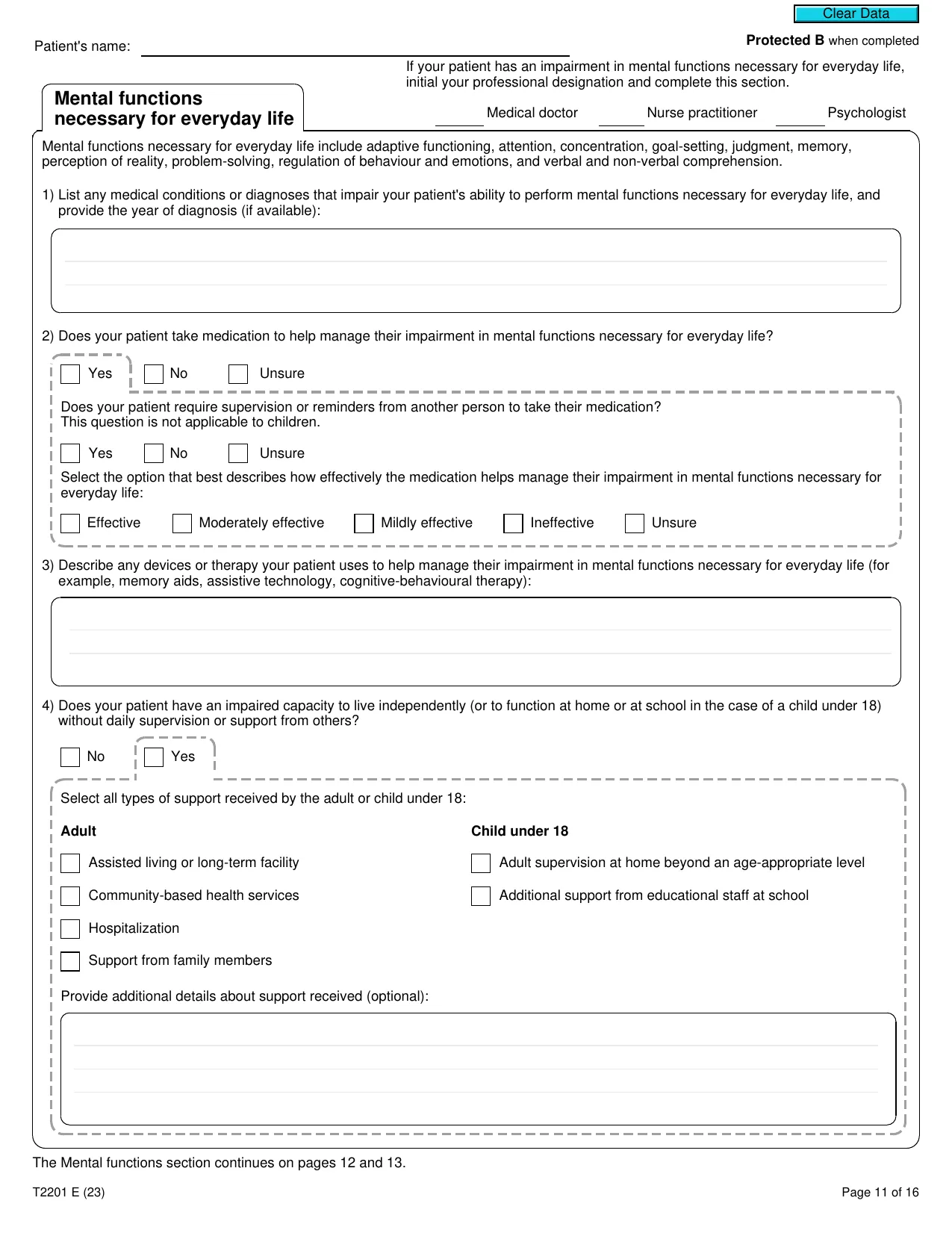
Patient's name:
If your patient has an impairment in mental functions necessary for everyday life,
initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Psychologist
Mental functions
necessary for everyday life
Mental functions necessary for everyday life include adaptive functioning, attention, concentration, goal-setting, judgment, memory,
perception of reality, problem-solving, regulation of behaviour and emotions, and verbal and non-verbal comprehension.
1) List any medical conditions or diagnoses that impair your patient's ability to perform mental functions necessary for everyday life, and
provide the year of diagnosis (if available):
2) Does your patient take medication to help manage their impairment in mental functions necessary for everyday life?
Yes
No
Unsure
Does your patient require supervision or reminders from another person to take their medication?
This question is not applicable to children.
Yes
No
Unsure
Select the option that best describes how effectively the medication helps manage their impairment in mental functions necessary for
everyday life:
Effective
Moderately effective
Mildly effective
Ineffective
Unsure
3) Describe any devices or therapy your patient uses to help manage their impairment in mental functions necessary for everyday life (for
example, memory aids, assistive technology, cognitive-behavioural therapy):
4) Does your patient have an impaired capacity to live independently (or to function at home or at school in the case of a child under 18)
without daily supervision or support from others?
No
Yes
Select all types of support received by the adult or child under 18:
Adult
Assisted living or long-term facility
Community-based health services
Hospitalization
Support from family members
Child under 18
Adult supervision at home beyond an age-appropriate level
Additional support from educational staff at school
Provide additional details about support received (optional):
The Mental functions section continues on pages 12 and 13.
T2201 E (23)
Page 11 of 16
Clear Data
Protected B
when completed
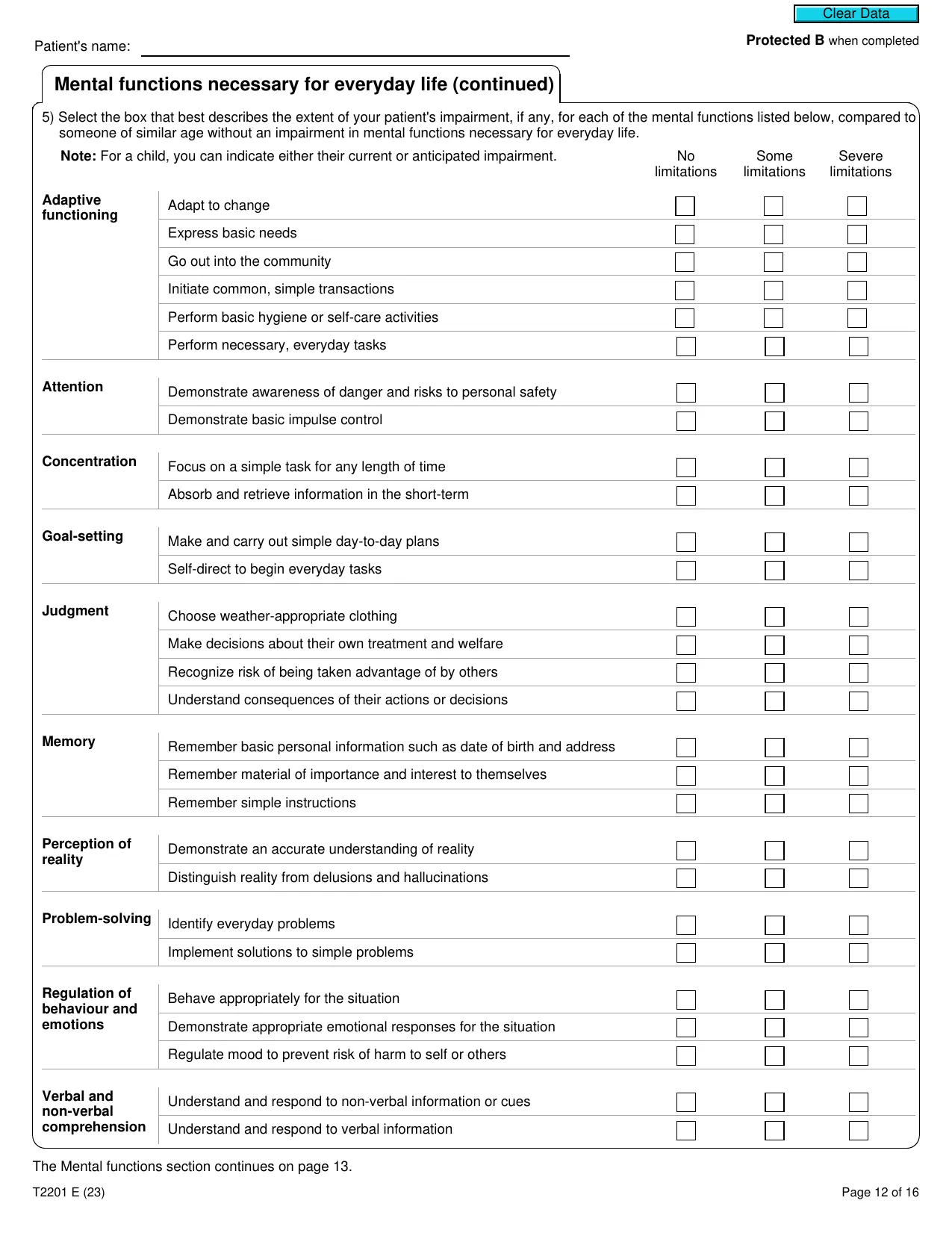
Patient's name:
Mental functions necessary for everyday life (continued)
5) Select the box that best describes the extent of your patient's impairment, if any, for each of the mental functions listed below, compared to
someone of similar age without an impairment in mental functions necessary for everyday life.
Note:
For a child, you can indicate either their current or anticipated impairment.
No
limitations
Some
limitations
Severe
limitations
Adaptive
functioning
Adapt to change
Express basic needs
Go out into the community
Initiate common, simple transactions
Perform basic hygiene or self-care activities
Perform necessary, everyday tasks
Attention
Demonstrate awareness of danger and risks to personal safety
Demonstrate basic impulse control
Concentration
Focus on a simple task for any length of time
Absorb and retrieve information in the short-term
Goal-setting
Make and carry out simple day-to-day plans
Self-direct to begin everyday tasks
Judgment
Choose weather-appropriate clothing
Make decisions about their own treatment and welfare
Recognize risk of being taken advantage of by others
Understand consequences of their actions or decisions
Memory
Remember basic personal information such as date of birth and address
Remember material of importance and interest to themselves
Remember simple instructions
Perception of
reality
Demonstrate an accurate understanding of reality
Distinguish reality from delusions and hallucinations
Problem-solving
Identify everyday problems
Implement solutions to simple problems
Regulation of
behaviour and
emotions
Behave appropriately for the situation
Demonstrate appropriate emotional responses for the situation
Regulate mood to prevent risk of harm to self or others
Verbal and
non-verbal
comprehension
Understand and respond to non-verbal information or cues
Understand and respond to verbal information
The Mental functions section continues on page 13.
T2201 E (23)
Page 12 of 16
Clear Data
Protected B
when completed
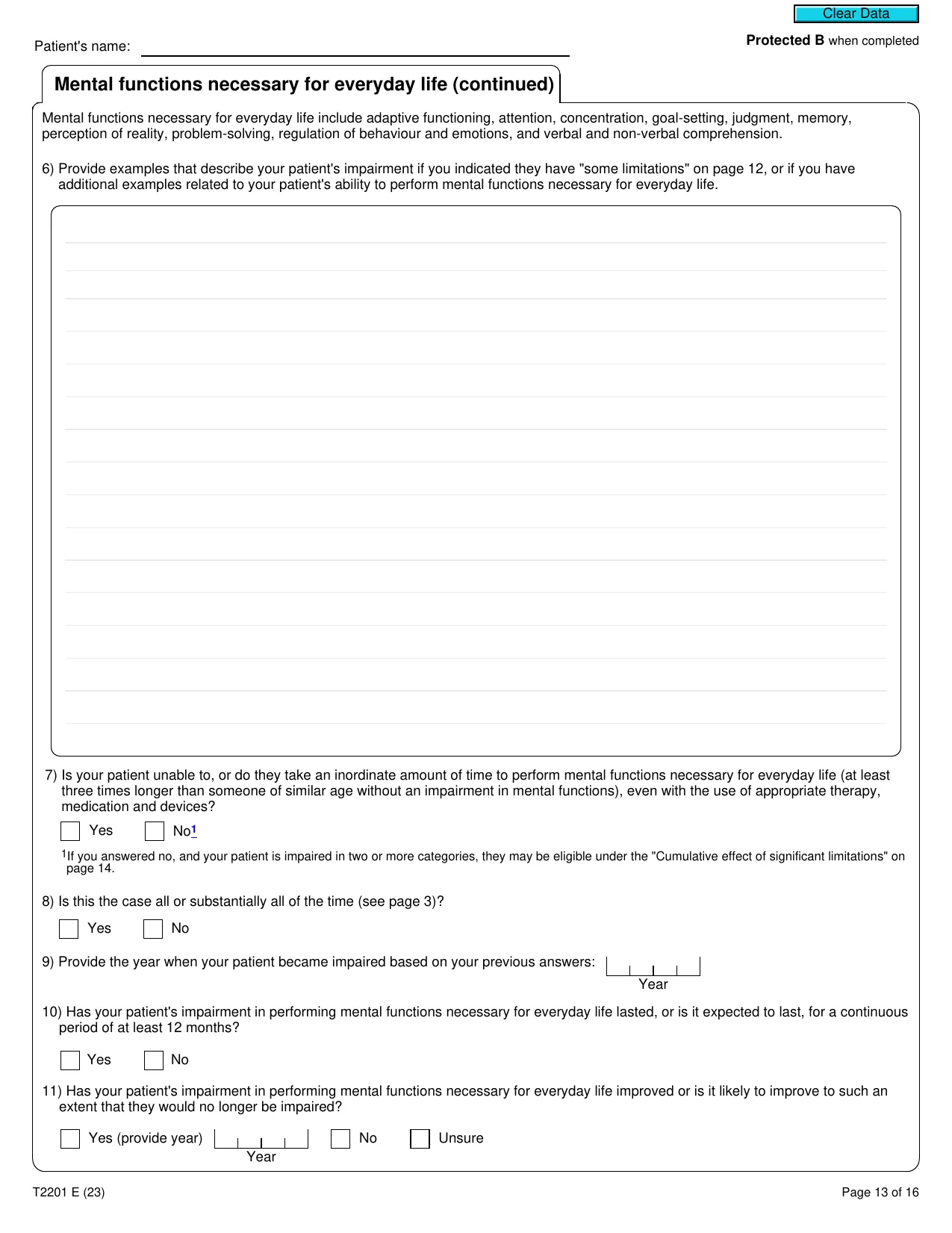
Patient's name:
Mental functions necessary for everyday life (continued)
Mental functions necessary for everyday life include adaptive functioning, attention, concentration, goal-setting, judgment, memory,
perception of reality, problem-solving, regulation of behaviour and emotions, and verbal and non-verbal comprehension.
6) Provide examples that describe your patient's impairment if you indicated they have "some limitations" on page 12, or if you have
additional examples related to your patient's ability to perform mental functions necessary for everyday life.
7) Is your patient unable to, or do they take an inordinate amount of time to perform mental functions necessary for everyday life (at least
three times longer than someone of similar age without an impairment in mental functions), even with the use of appropriate therapy,
medication and devices?
Yes
No
1
1
If you answered no, and your patient is impaired in two or more categories, they may be eligible under the "Cumulative effect of significant limitations" on
page 14.
8) Is this the case all or substantially all of the time (see page 3)?
Yes
No
9) Provide the year when your patient became impaired based on your previous answers:
Year
10) Has your patient's impairment in performing mental functions necessary for everyday life lasted, or is it expected to last, for a continuous
period of at least 12 months?
Yes
No
11) Has your patient's impairment in performing mental functions necessary for everyday life improved or is it likely to improve to such an
extent that they would no longer be impaired?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 13 of 16
Clear Data
Protected B
when completed
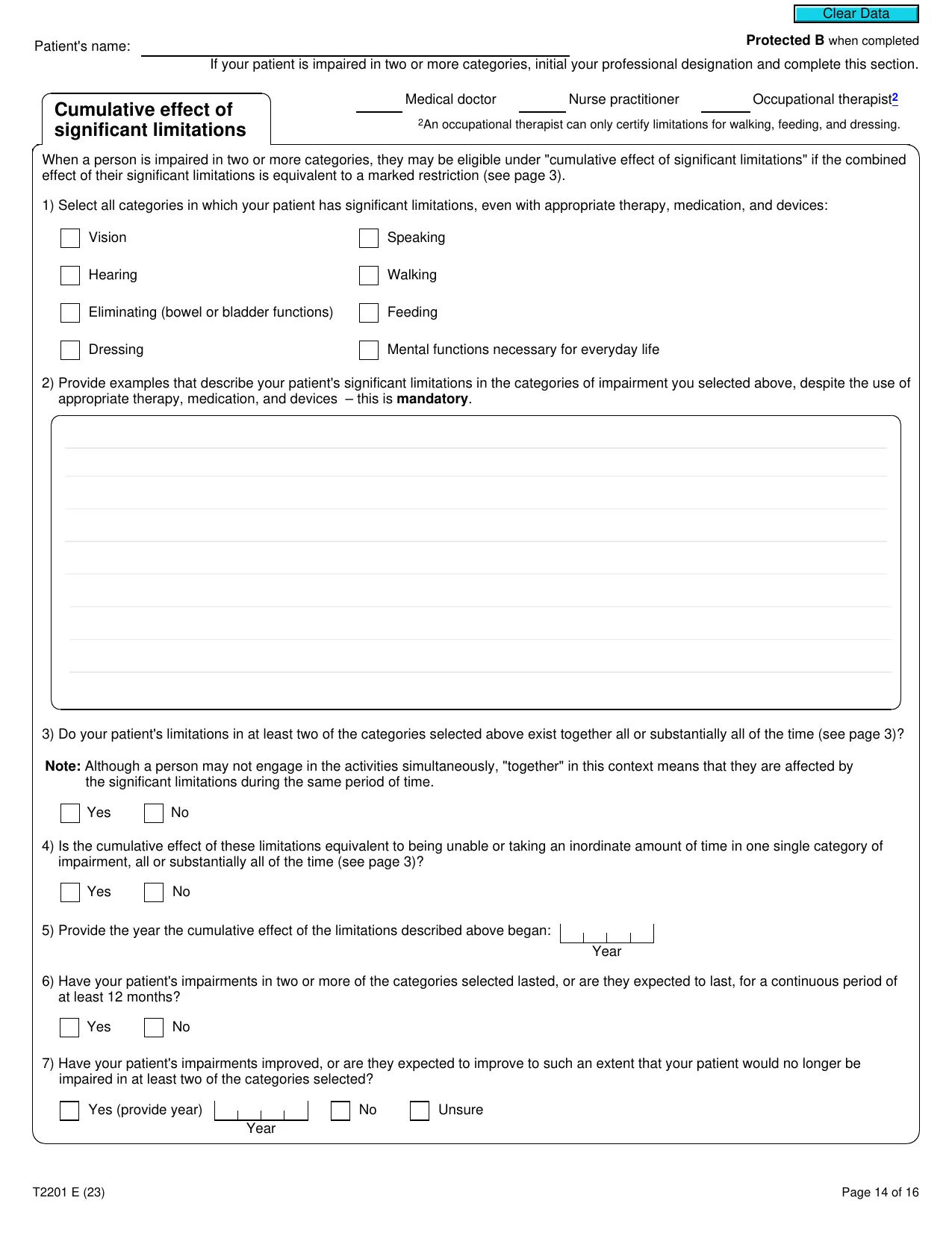
Patient's name:
If your patient is impaired in two or more categories, initial your professional designation and complete this section.
Medical doctor
Nurse practitioner
Occupational therapist
2
2
An occupational therapist can only certify limitations for walking, feeding, and dressing.
Cumulative effect of
significant limitations
When a person is impaired in two or more categories, they may be eligible under "cumulative effect of significant limitations" if the combined
effect of their significant limitations is equivalent to a marked restriction (see page 3).
1) Select all categories in which your patient has significant limitations, even with appropriate therapy, medication, and devices:
Vision
Speaking
Hearing
Walking
Eliminating (bowel or bladder functions)
Feeding
Dressing
Mental functions necessary for everyday life
2) Provide examples that describe your patient's significant limitations in the categories of impairment you selected above, despite the use of
appropriate therapy, medication, and devices – this is
mandatory
.
3) Do your patient's limitations in at least two of the categories selected above exist together all or substantially all of the time (see page 3)?
Note:
Although a person may not engage in the activities simultaneously, "together" in this context means that they are affected by
the significant limitations during the same period of time.
Yes
No
4) Is the cumulative effect of these limitations equivalent to being unable or taking an inordinate amount of time in one single category of
impairment, all or substantially all of the time (see page 3)?
Yes
No
5) Provide the year the cumulative effect of the limitations described above began:
Year
6) Have your patient's impairments in two or more of the categories selected lasted, or are they expected to last, for a continuous period of
at least 12 months?
Yes
No
7) Have your patient's impairments improved, or are they expected to improve to such an extent that your patient would no longer be
impaired in at least two of the categories selected?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 14 of 16
Clear Data
Protected B
when completed
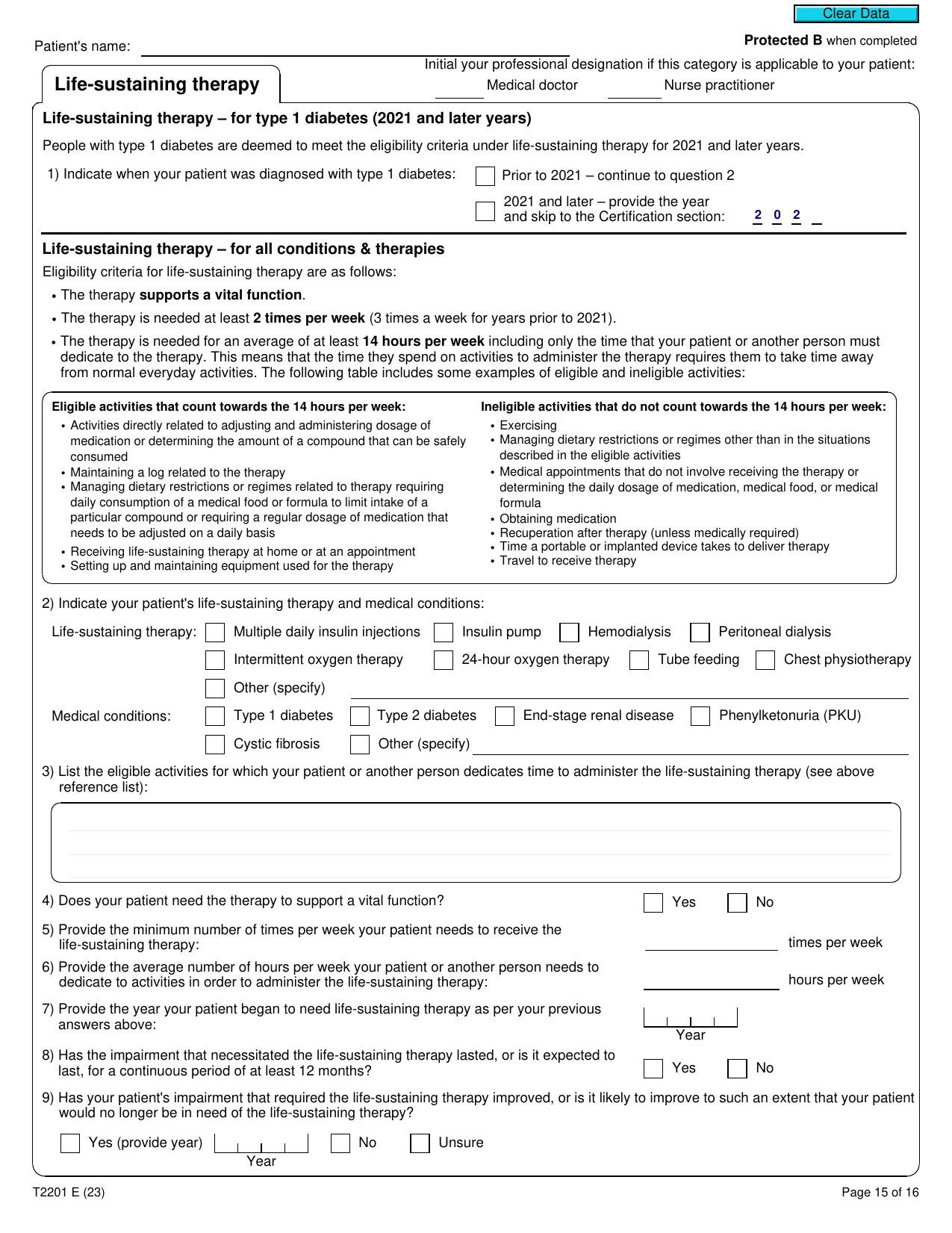
Patient's name:
Initial your professional designation if this category is applicable to your patient:
Medical doctor
Nurse practitioner
Life-sustaining therapy
Life-sustaining therapy – for type 1 diabetes (2021 and later years)
People with type 1 diabetes are deemed to meet the eligibility criteria under life-sustaining therapy for 2021 and later years.
1) Indicate when your patient was diagnosed with
type 1 diabetes:
Prior to 2021 – continue to question 2
2021 and later – provide the year
and skip to the Certification section:
Life-sustaining therapy – for all conditions & therapies
Eligibility criteria for life-sustaining therapy are as follows:
•
The therapy
supports a
vital function
.
•
The therapy is needed at least
2 times per week
(3 times a week for years prior to 2021).
•
The therapy is needed for an average of at least
14 hours per week
including only the time that your patient or another person must
dedicate to the therapy. This means that the time they spend on activities to administer the therapy requires them to take time away
from normal everyday activities. The following table includes some examples of eligible and ineligible activities:
Eligible activities that count towards the 14 hours per week:
• Activities directly related to adjusting and administering dosage of
medication or determining the amount of a compound that can be safely
consumed
• Maintaining a log related to the therapy
• Managing dietary restrictions or regimes related to therapy requiring
daily consumption of a medical food or formula to limit intake of a
particular compound or requiring a regular dosage of medication that
needs to be adjusted on a daily basis
• Receiving life-sustaining therapy at home or at an appointment
• Setting up and maintaining equipment used for the therapy
Ineligible activities that do not count towards the 14 hours per week:
• Exercising
• Managing dietary restrictions or regimes other than in the situations
described in the eligible activities
• Medical appointments that do not involve receiving the therapy or
determining the daily dosage of medication, medical food, or medical
formula
• Obtaining medication
• Recuperation after therapy (unless medically required)
• Time a portable or implanted device takes to deliver therapy
• Travel to receive therapy
2) Indicate your patient's life-sustaining therapy and medical conditions:
Life-sustaining therapy:
Multiple daily insulin injections
Insulin pump
Hemodialysis
Peritoneal dialysis
Intermittent oxygen therapy
24-hour oxygen therapy
Tube feeding
Chest physiotherapy
Other (specify)
Medical conditions:
Type 1 diabetes
Type 2 diabetes
End-stage renal disease
Phenylketonuria (PKU)
Cystic fibrosis
Other (specify)
3) List the eligible activities for which your patient or another person dedicates time to administer the life-sustaining therapy (see above
reference list):
4) Does your patient need the therapy to support a vital function?
Yes
No
5) Provide the minimum number of times per week your patient needs to receive the
life-sustaining therapy:
times per week
6) Provide the average number of hours per week your patient or another person needs to
dedicate to activities in order to administer the life-sustaining therapy:
hours per week
7) Provide the year your patient began to need life-sustaining therapy as per your previous
answers above:
Year
8) Has the impairment that necessitated the life-sustaining therapy lasted, or is it expected to
last, for a continuous period of at least 12 months?
Yes
No
9) Has your patient's impairment that required the life-sustaining therapy improved, or is it likely to improve to such an extent that your patient
would no longer be in need of the life-sustaining therapy?
Yes (provide year)
Year
No
Unsure
T2201 E (23)
Page 15 of 16
Clear Data
2
0
2
Protected B
when completed
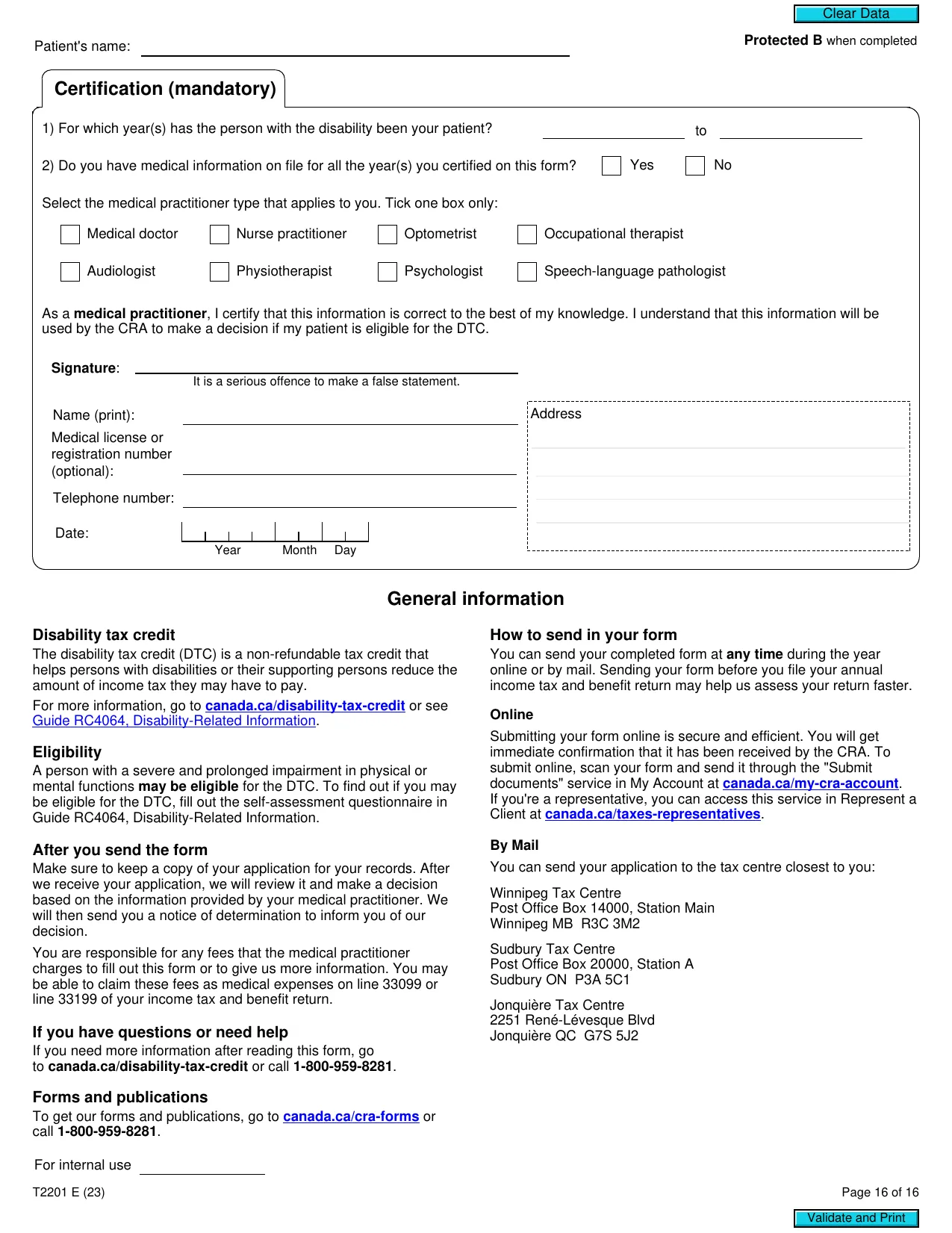
Patient's name:
Certification (mandatory)
1) For which year(s) has the person with the disability been your patient?
to
2) Do you have medical information on file for all the year(s) you certified on this form?
Yes
No
Select the medical practitioner type that applies to you. Tick one box only:
Medical doctor
Nurse practitioner
Optometrist
Occupational therapist
Audiologist
Physiotherapist
Psychologist
Speech-language pathologist
As a
medical practitioner
, I certify that this information is correct to the best of my knowledge. I understand that this information will be
used by the CRA to make a decision if my patient is eligible for the DTC.
Signature
:
It is a serious offence to make a false statement.
Name (print):
Medical license or
registration number
(optional):
Telephone number:
Date:
Year Month Day
Address
General information
Disability tax credit
The disability tax credit (DTC) is a non-refundable tax credit that
helps persons with disabilities or their supporting persons reduce the
amount of income tax they may have to pay.
For more information, go to
canada.ca/disability-tax-credit
or see
Guide RC4064, Disability-Related Information
.
Eligibility
A person with a severe and prolonged impairment in physical or
mental functions
may be eligible
for the DTC. To find out if you may
be eligible for the DTC, fill out the self-assessment questionnaire in
Guide RC4064, Disability-Related Information.
After you send the form
Make sure to keep a copy of your application for your records. After
we receive your application, we will review it and make a decision
based on the information provided by your medical practitioner. We
will then send you a notice of determination to inform you of our
decision.
You are responsible for any fees that the medical practitioner
charges to fill out this form or to give us more information. You may
be able to claim these fees as medical expenses on line 33099 or
line 33199 of your income tax and benefit return.
If you have questions or need help
If you need more information after reading this form, go
to
canada.ca/disability-tax-credit
or call
1-800-959-8281
.
Forms and publications
To get our forms and publications, go to
canada.ca/cra-forms
or
call
1-800-959-8281
.
How to send in your form
You can send your completed form at
any time
during the year
online or by mail. Sending your form before you file your annual
income tax and benefit return may help us assess your return faster.
Online
Submitting your form online is secure and efficient. You will get
immediate confirmation that it has been received by the CRA. To
submit online, scan your form and send it through the "Submit
documents" service in My Account at
canada.ca/my-cra-account
.
If you're a representative, you can access this service in Represent a
Client at
canada.ca/taxes-representatives
.
By Mail
You can send your application to the tax centre closest to you:
Winnipeg Tax Centre
Post Office Box 14000, Station Main
Winnipeg MB R3C 3M2
Sudbury Tax Centre
Post Office Box 20000, Station A
Sudbury ON P3A 5C1
Jonquière Tax Centre
2251 René-Lévesque Blvd
Jonquière QC G7S 5J2
For internal use
T2201 E (23)
Page 16 of 16
Validate and Print
Clear Data